CDI’S COVID-19 CLINICAL SUPPORT AND RESEARCH: A Scientific Update from Dr. Perlin
May 07, 2020
By Dr. David Perlin, chief scientific officer and senior vice president
The CDI was formally established in May 2019 with a fundamental mission to conduct “science with clinical impact” by translating in real-time insights from molecular and cellular science to improve patient outcomes, especially in cancer and infectious diseases. CDI science is guided by unmet medical need and is intended to address clinical urgency. There has been no greater challenge posed to patient and community health than COVID-19. Despite being less than one year old as a research enterprise, the CDI’s scientists and staff members, including experts in global infectious diseases, embraced this unprecedented challenge. They have played a critical role in impacting clinical care through development of novel diagnostics, improved antiviral therapy, and support of numerous clinical trial regimens. CDI scientists are also studying the biology of the virus, host factors that impact disease progression, and discovery and development of novel drug candidates.
CLINICAL SUPPORT
Rapid Molecular Testing of Virus. Yanan Zhao, M.D., Ph.D., and David Perlin, Ph.D., developed a highly accurate molecular assay for the rapid detection of COVID-19, which captured the best detection elements of tests developed by the CDC and WHO. This novel test was implemented in the Clinical Laboratory Improvement Amendments (CLIA)-approved high complexity molecular laboratory at Hackensack University Medical Center. It was approved for use with patients on March 12 by the NJ Department of Health under the FDA Emergency Use Authorization for COVID-19. Importantly, at the time, implementation of this test reduced delays in reporting sample results from 5-7 days to just a few hours, and it proved critical to diagnose and properly manage critically ill patients. Most prominently, it allowed emergency staff to triage patients more effectively by mobilizing the critical care infrastructure, especially negative-pressure isolation rooms, and helping healthcare professionals manage patients safely.
It was the first rapid test to be approved and implemented by a hospital system in New Jersey during the epidemic. The test has now been used to diagnose more than 2,500 hospitalized patients. This rapid bench- to-bed approach, which involved molecular assay development, test validation, implementation and operationalization, was a team effort between CDI scientists, David Chow, M.D., (Pathology and CDI) and members of the HUMC molecular lab. In addition to the clinical lab staff, more than a dozen CDI researchers volunteered to help run the test in the hospital. The test was licensed for commercial development to T2 Diagnostics. The media covered the developments:
Serology for Convalescent Therapy Program (CTP). For most COVID-19 patients, successful clinical outcome requires control of viral replication and either a prevention or control of destructive inflammatory responses (cytokine storm) that may arise following tissue damage. The lack of an effective and reliable antiviral agent has led to the use of convalescent therapy to control viral replication. This classical approach to control infection in the absence of an effective treatment has been used in recent decades to treat infections in patients due to Ebola, SARS-CoV-1, MERS, and now SARS CoV-2. The basic principle is that patients who recover from infection do so because they mount a strong antibody response that overcomes the infecting pathogen. These antibodies can be measured in the serum of blood from recovered patients and are presumed to kill or block the pathogen from further damage to the body. This killing potential, and in the case of SARS-CoV-2 antiviral activity can be transferred from a recovered donor in the form of blood plasma by transfusing a seriously ill patient to help the body fight off the disease. This type of antiviral therapy is safe, but its efficacy very much depends on clinical disease manifestation, the antiviral potential of antibodies in the transferred plasma, and the status of the host immune system. There is a national program for this therapy that is FDA approved and being led by the Mayo Clinic. For donors to qualify, their serum must contain antibodies at a certain threshold. The problem with this approach is that we don’t know what the correct threshold level is for a successful clinical outcome, as each recovered patient/donor mounts a different antibody response in terms of quantity and antiviral potency.HUMC Convalescent Therapy. Our approach has been to attack the problem of antiviral therapy as we would drug treatment for any infectious agent. The drug must be delivered to the site of infection at the appropriate drug level and potency for a sustainable duration to have a successful outcome. Many drugs fail in clinical trials because they are not properly dosed to reach this target level. To address this treatment principle for our patients, Michele Donato, M.D.,, a world renowned transplant expert at Hackensack Meridian Health’s John Theurer Cancer Center, developed an alternative protocol that maximizes the amount and potency of antiviral antibodies delivered to each patient. The protocol has been approved under an Investigational New Drug (IND) designation from the FDA.
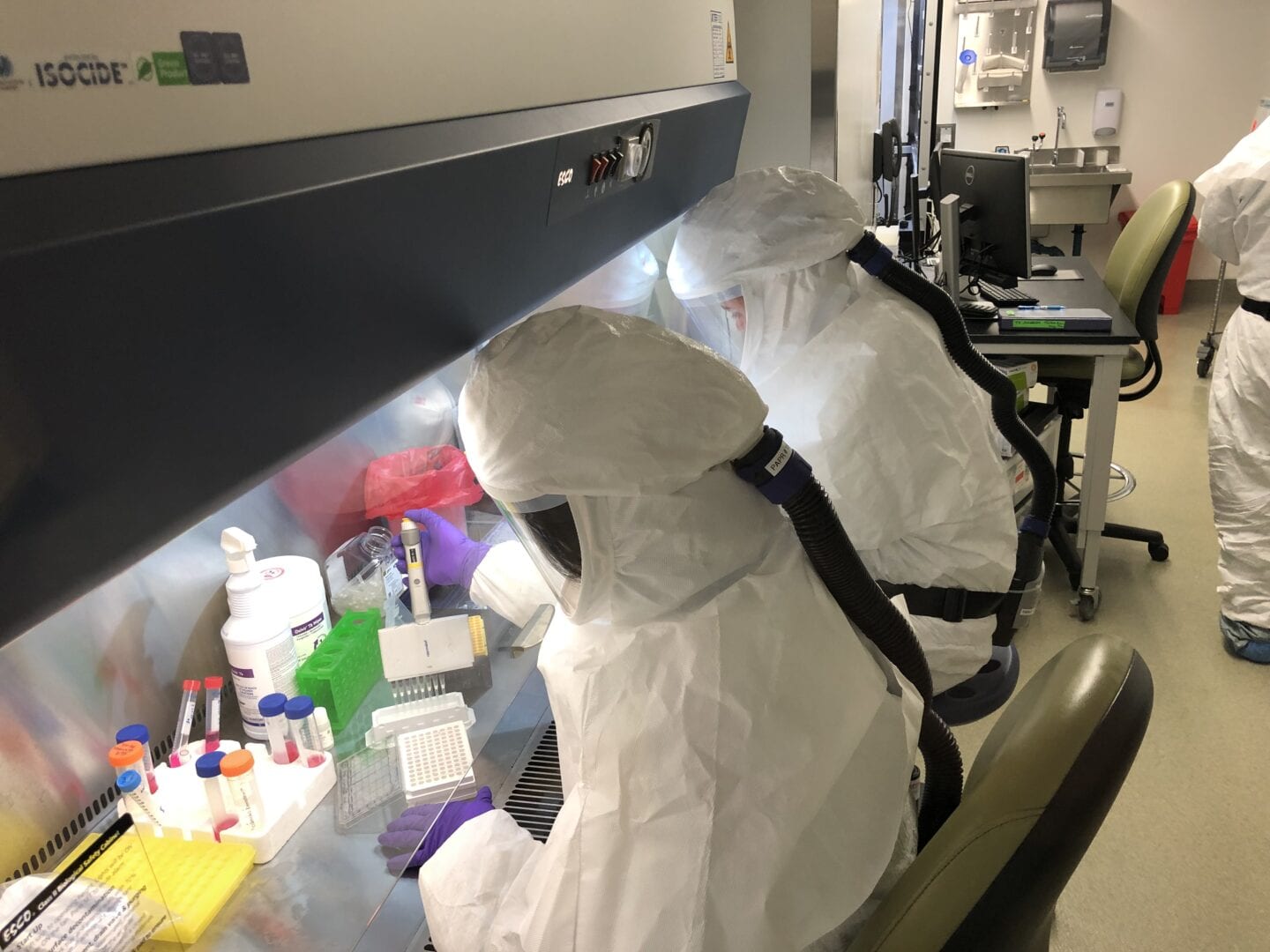
A key component of this therapy is the identification of recovered patient/donors with high titers of neutralizing antibodies that kill or disable the virus. The CDI screening program, led by Dr. Perlin and Steven Park, has been actively evaluating potential donors by performing a detailed assessment of Immunoglobin G (IgG) and Immunoglobin M (IgM) antibodies to identify the best donors for Convalescent Plasma therapy trials. We have more than 6,000 donors who have contacted us for this study. As expected, we observe a range of titers from weak or no antibody responses to highly neutralizing IgG at dilutions exceed 1:10:000. In this program, we are looking for the subset of potential donors with supra-high levels of neutralizing antibodies based initially on titers directed against the SARS-CoV-2 Spike RBD region. This initial screening work was greatly aided by the support of colleagues from the group of Dr. Florian Krammer at the Mount Sinai School of Medicine. Once high-titer sera are identified, we perform detailed antibody neutralization (protection) assays in a cytopathic virus challenge assay involving high exposures of SARS-CoV-2 with susceptible cells under biosafety level 3 (BSL-3) containment.Finally, as part of the convalescent plasma therapy clinical trial, the CDI, led by Robert Korngold, Ph.D., and Martin Gengenbacher, Ph.D., are providing immune profiling involving a variety of antivirals and anti-inflammatory agents to understand changes in T cell populations (CD4 +, CD8 + CD25 +), other lymphocytes, NK cells, cytokines and chemokines, etc.
HMH COVID-19 Universal Real-Time Database. In any epidemic or new disease, the accurate and real-time tracking of clinical data is essential to understand trends, clusters, treatment, and other important disease features and manifestations. Stuart Goldberg, M.D., and Andrew Ip, M.D., have established one of the most comprehensive clinical data bases that includes more than 450 clinical features for 3000 COVID-19 patients. This rich source of clinical data is being used by CDI scientists to identify COVID-19 patient cohorts that can then be studied in detail.
Support of Clinical Trials at HMH. A wide variety of Pharmaceutical-Sponsored and Investigator-Sponsored clinical trials are underway at various Hackensack Meridian Health hospitals since the start of the epidemic in New Jersey. These trials involve national studies of antivirals like Remdesivir, hydroxychloroquine, and NK cells, as well as studies of anti-inflammatory drug affecting IL-6, IL-1 and Il-2, and others. CDI scientists play a vital support role in many studies by evaluating virus status, and downstream assessment of immunologic markers.
ADVANCING COVID-19 SCIENCE
Drug Discovery. Pharmaceutical, biotech companies and academic discovery groups have partnered with CDI to develop new drug candidates against COVID-19, and other coronaviruses. Utilizing a SARS-CoV-2 viral pathogenic screening assay that mimics viral infection of host cells in our Biosafety Level 3 lab suite, Dr. Perlin and Steven Park lead a team including Megan Mitchell, Ph.D., that has evaluated more than 200 compounds representing approved drugs, drug candidates in late-stage clinical development as antivirals, and as well as new chemical classes. Many of these compounds have the potential to be repurposed rapidly for clinical trials. This work is being performed as part of an NIH Center of Excellence in Translational Research focused on novel anti-infective development.
Biorepository (Bio-R). It was recognized at the earliest stage of the COVID-19 epidemic that organized collection and processing of biological specimens from hospitalized patients linked to clinical data would be essential to understand this disease. The Bio-R, led by Dr. Chow and Yael Kramer, has been diligently collecting thousands of specimens from patients after obtaining informed consent for those specimens to be used for research purposes. Basic categories of patient specimens based on clinical disease states have been collected and include patients who were hospitalized, critically-ill and in the ICU with or without mechanical ventilation. Specimen types include: nasal and oropharyngeal swabs, extracted nucleic acid, blood, serum, respiratory fluids, stool and indwelling devices. The hard work of consenting and collecting specimen has been performed by the Bio-R team, the team of Chinwe Ogedegbe, M.D., group in the Emergency Department at HUMC and Marygrace Zetkulic, M.D., and Medical Residents within the HUMC ICU.
Genomics and Beyond. The CDI has partnered with the New York Genome Center (NYGC) as part of a large consortium of mostly New York metropolitan area universities and hospitals. The objective is to share data in real-time about emerging science related to COVID-19, and to exploit genomics and genetic sequencing to explore key questions of virus microevolution, host susceptibility and disease progression. Specific CDI programs include:
- Large scale full-length viral sequencing to determine viral evolution and spread across the community and within the individual (e.g. oral, nasal, lung, GI tract) Barry Kreiswirth, Ph.D., and Liang Chen, Ph.D.
- Whole-genome germline sequencing and immune repertoire sequencing of affected individuals, focused on extreme phenotypes to examine host factors and immune responses - Benjamin Tycko, M.D., Ph.D.
- Single-cell sequencing to examine tissue responses and provide a genome variation of expression context for viral responses - NYGC.
- Establishment of a data commons at the NYGC for the research network so that full availability of data to investigators can be provided - Andrew Ip, M.D.
- Lung and GI tract microbiome of disease cohorts - Rena Feinman, Ph.D.
- Evaluation of secondary bacterial and fungal infections in COVID-19 patients - Dr. Kreiswirth and Milena Kordalewska, Ph.D.
- Use of endothelial stem cells to repair damaged tissue in revolvered patients - Jason Butler, Ph.D.
- Assessment of exosomes and microRNA populations in COVID-19 patients –Olivier Loudig, Ph.D., and Dr. Mitchell
- Role of membrane sphingolipids in COVID-19 disease - Claire Carter, Ph.D.
